Clinical presentation
Feline oral squamous cell carcinoma (FOSCC) is a cancer of the lining of the mouth. The most common age of diagnosis is 10-12 years of age. There is no known breed predilection. FOSCC most commonly looks like an area of deep ulceration (involving bone) or expansile mass in one focal area of the gums or gingiva of the upper or lower jaw. FOSCC can also occur on or under the tongue and in this location more commonly appears as an expansile mass.
Less common locations of FOSCC include the cheek, back of the throat (pharynx), or tonsils. Cats with FOSCC commonly lose weight, have a pickier appetite, exhibit pain on opening the mouth, drool (often with blood tinged saliva) and have bad breath. Depending on the location of the tumor, loose teeth (if tumor is in the jaw), deviation of the tongue to one side (if tumor is in the tongue), swollen face, nose bleeds, or eye bulging may also be seen.
Other non-specific signs such as hiding, lethargy may also be seen. These signs are not specific to FOSCC as they can also occur with other common problems in cats such as dental problems, kidney disease or infections.
Causes
Increasing age is the strongest risk factor for developing FOSCC. Other risk factors include eating canned tuna or canned cat foods, or exposure to second-hand tobacco smoke. Most studies have not found viral infections to be a common risk factor.
Differential Diagnosis
FOSCC can look like non-cancerous conditions such as severe gingivitis / stomatitis (dental disease) or an eosinophilic granuloma or ulcer. FOSCC is the most common oral tumor in cats but other tumors can mimic FOSCC, including fibrosarcoma, melanoma and lymphoma.
Diagnosis
If a cat is under anesthesia for a dental we recommend biopsy of any concerning and abnormal tissue. FOSCC may also be diagnosed in many cases with a fine needle aspirate under sedation. It is always recommended that any aspirate or biopsied tissue be submitted to a pathologist for review.
Additional diagnostics
Routine bloodwork (CBC, chemistry and urinalysis) is always recommended when an animal is diagnosed with cancer. Thoracic radiographs (x-rays) should be done to determine if there is evidence of lung metastasis (cancer that has spread to the lungs). Computed tomography (CT scan) is the preferred imaging method to evaluate the local and distant extent of the tumor (staging). A CT scan can be done of the head to determine if the mass is invading the deeper tissues, of the neck to determine if there is suspected metastasis to the lymph nodes deep in the neck, of the chest to determine if there are metastases to the lungs, and abdomen to determine if there is any evidence of another unrelated tumor or abnormality. A CT is necessary in the majority of cases to plan for surgery or radiation therapy. Aspirates of both the left and right mandibular lymph nodes and any other enlarged lymph nodes are recommended prior to treatment. It is possible to have metastatic lymph nodes even if the lymph nodes feel normal on exam and look normal on a CT scan. The diagnostic plan takes into account many factors and may differ in each case.
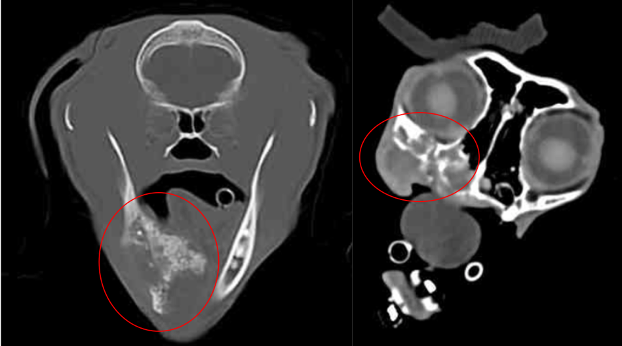
Courtesy of the University of Missouri
Left: FOSCC tumor causing destruction and production of bone in the mandible. The mass extends under the tongue.
Right: FOSCC tumor in the maxilla causing destruction of the bones under the eye and extends to the nasal passages.
Clinical course
At the time of diagnosis the majority of cats do not have evidence of metastasis and thus treatment is focused on the local discomfort from the tumor in the mouth. Local treatments could include surgery (if possible) or radiation therapy. If local treatment has been successful and there is no longer evidence of the tumor or the tumor is substantially decreased in size systemic treatment such as IV chemotherapy can be given to decrease the risk of metastasis. With local treatment the majority of cats will have significant improvement of their clinical signs but this is typically temporary and the tumor and signs return after a few months of ending treatment. Cats with FOSCC are typically euthanized due to oral discomfort from their tumor.
Treatment
Surgery
The presence of a very extensive tumor at the time of diagnosis often would require a radical resection of a large part of the jaw, making surgery morbid and not feasible. However, if the tumor is small, is in a location amenable to surgery and owners understand the surgical risks, surgery may be a good option. If surgical margins are incomplete (tumor cells seen at the edge of the biopsy sample under the microscope) or narrow, follow-up radiation therapy may be recommended to decrease the risk of local recurrence. There is a risk that after surgery a feeding tube (esophagus or stomach) may be required after surgery. In most cases this is temporary. In ~12% of cases treated with removal of half of the mandible (lower jaw), tube feeding may be permanently required and this eventuality cannot be predicted prior to surgery. Prior to determining if surgery is a good option the surgeon will need to review the CT scan and perform a sedated oral exam of the patient.
Palliative medical care (hospice)
The goal of palliative care is to make the patient feel more comfortable without the risk of significant side effects. Palliative care could include anti-inflammatories (e.g. Metacam or Onsior in cats that have adequate kidney function or, alternatively, prednisolone), pain control (e.g. buprenorphine, gabapentin or Metacam), appetite stimulants (e.g. mirtazapine, steroids), antibiotics (if the mass is infected) and/or IV bisphosphonates (to decrease bone pain).
Palliative care is not expected to make the tumor shrink in size and tumor progression is expected with palliative care.
Oral Palladia
This is an oral growth inhibitor chemotherapy drug that is given at home 3 times per week. Since it is chemotherapy this pill cannot be crushed, split or mixed into food. Efficacy is debatable but complete and partial responses have been seen in approximately 13% of cases in a previous small study. The most common side effects from Palladia in cats include decreased appetite, vomiting and diarrhea. Because of a low chance of efficacy and risk of side effects, this is not a commonly used treatment option. Palladia is most commonly administered in conjunction with a non-steroidal anti-inflammatory on alternating days.
Radiation therapy and chemotherapy
Radiation therapy is generally directed at one location in the body. Because radiation must be precisely delivered to avoid significant radiation side effects, a CT is necessary to make a radiation plan. This CT must be positioned in a special way and thus needs to be done with the treating oncologist. Radiation therapy works by damaging the DNA of tumor cells. Because cancer cells may either be dividing or laying dormant, the effects of radiation can be seen at various times following administration. It takes multiple treatments to cause DNA damage to accumulate within a cell. Once a cell has been damaged beyond repair, cell death will occur when it attempts to divide. Because of the time gap from damage to division, tumors can shrink slowly over weeks to months, or sometimes simply stop growing.
When oncologists plan radiation, the total dose to be administered to the tumor is divided into smaller treatments called fractions. Fractionation allows the normal tissues to better tolerate the radiation. Treatment plans for FOSCC vary substantially depending on many patient, owner and attending veterinarian factors. Common treatment options at the University of Missouri include daily to twice daily radiation therapy for approximately 2-3 weeks (accelerated protocol).
Short term (acute or early) and long term (chronic or late) radiation effects may occur. Early effects will happen in all animals to some extent and will heal within 3 to 4 weeks following radiation. Early effects begin during the second half of a course of radiation treatment and will be at their peak (worst) toward the end or just after completion of a course of radiation therapy. Late effects are uncommon or rare but are permanent and occur more than one year following radiation treatment. Early effects that will happen but will resolve with time and oral medications (e.g. pain medications and anti-inflammatories) include mucositis (inflammation of the oral mucosa), alopecia (hair loss), temporary dry eye, and desquamation (scaling and loss of the superficial layer of skin). A feeding tube (through the neck or abdominal wall) may be required during or after radiation therapy while the early effects heal. Late effects can include osteonecrosis causing an oronasal fistula (death of a piece of bone causing communication of the nasal and oral cavities), permanent hair loss, cataracts, delayed healing from corneal ulcers, permanent dry eye and secondary cancers.
Intravenous chemotherapy can increase the efficacy of radiation therapy but can increase side effects. The attending veterinary oncologist will help determine if and when adding chemotherapy is appropriate.
In most cats (~75%), radiation therapy with chemotherapy will shrink the tumor but is generally considered to be palliative because the tumor is likely to recur after a few months of ending radiation therapy.
Prognosis
The prognosis for most cats with FOSCC is poor even with treatment. Most cats with FOSCC succumb to their disease within the first year of diagnosis and the 1-year survival rate is estimated to be less than 10%. But cats that have their tumors surgically removed with complete margins are more likely to have long term survival (median survival times of > 1 year). The most important prognostic factor is early identification of this tumor when it is small. Cats with FOSCC tumors in surgically amenable locations such as the mandible, cheek and tonsils may have a better prognosis than FOSCC tumors in other locations. Median survival time (50% did better and 50% did worse in the study) of cats treated with radiation therapy +/- chemotherapy has been estimated to be approximately 3-6 months. Median survival time for cats on palliative care is ~1.5-2 months.
Prevention
At this time there are no known direct causes of FOSCC. Limiting exposures to known risk factors would be advised. Routine visits with a veterinarian every 6 months would be recommended in general for geriatric cats if possible. During these visits a thorough physical exam may detect FOSCC or other cancers and routine bloodwork may detect common chronic diseases in cats (e.g. diabetes, kidney disease, hyperthyroidism, etc). Early diagnosis (when the tumor is small) is expected to improve the prognosis for cats that are treated for their FOSCC.
Active areas of research in FOSCC
Research on new treatment options have evaluated the efficacy of injecting chemotherapy or radiation therapy into the tumor, stereotactic radiation therapy and targeted inhibitors (e.g. fatty acid synthase) but more research is needed to determine if these are more effective treatment options than current available options. Research on causes of FOSCC have evaluated viral causes and environmental exposure.
How you can help with research in FOSCC
If your cat has been diagnosed with FOSCC or you had a cat that was diagnosed with FOSCC after January 2010 please contact the University of Missouri to see how you can participate in research that can help. You can also help by forwarding this information to anyone you know that has/had a cat with FOSCC that was diagnosed after January 2010.
Resources